Explanation of Benefits

Explanation of Benefits
This Is Not A Bill. So, What is This?
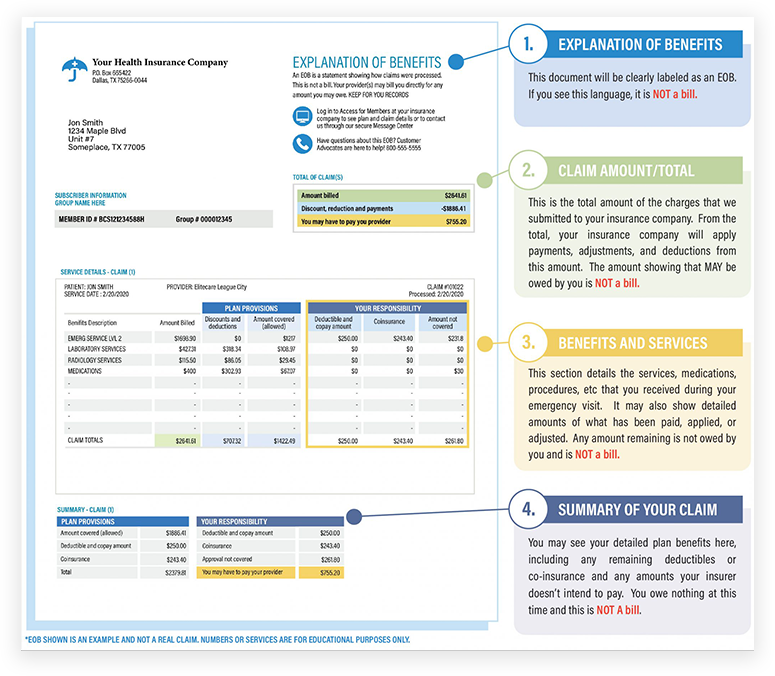
You may receive an Explanation of Benefits (EOB) from your insurance company shortly after your emergency visit. We want you to understand one very important fact that will be reiterated throughout this page. An EOB is NOT a bill. Do not be concerned, do not worry… you do not owe anything at this time and you will NOT owe ANYTHING until you receive a bill from us -and it will be clearly labeled as such.
An EOB is a communication document from your insurance company informing you that the claim process has begun. Our billing representatives are communicating on your behalf with the insurer regarding the charges from your emergency visit. The claim process can take many months. When the process is complete, most patients owe significantly less than what is stated on the EOB, sometimes even nothing at all. If you have questions during the claim process, please don’t hesitate to call a friendly advocate at (281) 337-7500.
AN INSURANCE COMPANY’S “EXPLANATION OF BENEFITS” IS NOT A BILL!
When you get something from your health insurance company that looks like the image above…
IT IS NOT A BILL! DO NOT PAY IT!
IT IS NOT FROM Elitecare.
THEN WHAT IS AN “EXPLANATION OF BENEFITS” (“EOB”)?
(Hint-it is almost never helpful, almost never accurate or even an “explanation’?
An EOB is a standard document used by health insurance companies (“Insurers”) to communicate with patients. Here is what you need to understand when you get the EOB.
First, the EOB will state the medical services you received and identify the healthcare provider. This is done for their benefit so the Insurers can make sure you received the services the Insurers are being billed for. So far, so good.
Second, the EOB will state the gross charges for these services and how you and your plan will share the payment of those charges under your health insurance plan. If the healthcare provider is in-network with the insurance plan, the charges may already be adjusted to what will actually be owed and paid. In such case, the insurer can use the EOB as a tool showing you the savings you received by going to in-network healthcare facilities. Unfortunately, insurers do not extend this same courtesy to out-of-network healthcare providers.
Third, and unfortunately, the EOB is virtually worthless as an explanation if the healthcare provider is out-of-network, as EliteCare is with most plans. The simple reason the EOB is worthless is that insurers send out the EOB before the final amount to be deemed “allowable” and the final amount to be payable on the claim are determined.
Fourth, resolving the actual amount to be payable and paid by the insurer is complex and takes months – you will not be billed by EliteCare for any patient portion until the process is complete.
Fifth, at EliteCare you will never be “balanced billed” for more than what you owe based on (1) an agreed allowable amount (usually comparable to reasonable in-network charges) and (2) the amounts your insurance plan requires as co-insurance, co-pays and deductibles.
WARNING
some of our out-of-network competitors DO BALANCE BILL and that is one more reason why EliteCare is your best emergency care option.
WHY IS THE PROCESS SO COMPLEX AND WHY DOES IT TAKE SO LONG?
Hint – you do not need to read this unless you are interested in understanding the process.
Reason #1
Insurers are required to pay for emergency medical care at out-of-network facilities under the Affordable Care Act and Federal Law at benefit rates that are comparable to in-network rates – most insurers frequently fail to do so until the claim is appealed.
Reason #2
In almost all cases, EliteCare negotiates with the insurers (1) to set an appropriate discounted amount of our charges (an “allowable” amount) and (2) to make sure the insurer pays the maximum benefit you are entitled to receive under your plan – benefits that are comparable to in-network benefits. This takes time and effort – lots of time and effort It often involves appealing the insurer’s initial determination of benefits. This billing service is all part of our EliteCare service. As a result, you will ultimately owe far less than what is “displayed” on the initial EOB. The ultimate amount you will owe will be limited by the allowable amount we agree to with your insurer and the terms of your health insurance plan.
WHY DOESN’T EliteCare GO IN-NETWORK?
We would have to write a book to answer this question.
However, the biggest reason is that we are a small healthcare provider and most of the insurers do not offer us the same (or even similar) contracted rates that they offer to larger hospital systems. They do not want to add additional providers to their network and they do not want the increased access to emergency care that we provide. Thankfully, we dont exist to serve the insurance companies. We exist to serve our patients and our communities – and the vast majority of our patients love us and appreciate the better access to emergency care.
Patient Resources: